- Research
- Open access
- Published:
Clinical virtual simulation: predictors of user acceptance in nursing education
BMC Medical Education volume 24, Article number: 299 (2024)
Abstract
Background
Using virtual patients integrated in simulators expands students’ training opportunities in healthcare. However, little is known about the usability perceived by students and the factors/determinants that predict the acceptance and use of clinical virtual simulation in nursing education.
Objectives
To identify the factors/determinants that predict the acceptance and use of clinical virtual simulation in learning in nursing education.
Methods
Observational, cross-sectional, analytical study of the use of clinical virtual simulation in nursing to answer the research question: What factors/determinants predict the acceptance and use of a clinical virtual simulator in nursing education? We used a non-probabilistic sampling, more specifically a convenience sample of nursing degree students. The data were collected through a questionnaire adapted from the Technology Acceptance Model 3. In technology and education, the Technology Acceptance Model is a theoretical model that predicts the acceptance of the use of technology by users.
Results
The sample comprised 619 nursing students, who revealed mean values of perceived usefulness (M = 5.34; SD = 1.19), ease of use (M = 4.74; SD = 1.07), and intention to use the CVS (M = 5.21; SD = 1.18), in a Likert scale of seven points (1—the worst and 7 the best possible opinion).
This study validated the use of Technology Acceptance Model 3 adapted and tested the related hypotheses, showing that the model explains 62% of perceived utility, 32% of ease of use, and 54% of intention to use the clinical virtual simulation in nursing by nursing students. The adequacy of the model was tested by analysis of the direct effects of the relationships between the internal constructs (PU-BI, β = 0.11, p = 0.012; PEOU-BI, β = -0.11, p = 0.002) and the direct relations between some of the constructs internal to the Technology Acceptance Model 3 and the external determinants Relevance for learning and Enjoyability.
In the proposed model, the external constructs that best predicted perceived usefulness, ease of use, and behaviour intention to use the clinical virtual simulation in nursing were Relevance for learning and Enjoyability.
Conclusions
These study results allowed us to identify relevance for learning and enjoyability as the main factors/determinants that predict the acceptance and use of clinical virtual simulation in learning in nursing.
Introduction
The rapid transformation of society in recent decades and the technical and scientific advancements in health sciences continually challenge higher education institutions (HEIs) to innovate, develop, and implement new pedagogical methodologies that guarantee up-to-date and quality training. Translating knowledge into clinical practice has become one of the main challenges of the first decades of the twenty-first century in research and higher education in health [1, 2]. The higher education institutions have been systematically confronted with the difficulty of teaching central and structuring concepts of clinical practice and difficulty in translating these concepts into clinical practice [1, 2]. Since the 1950s, multiple pedagogical strategies have been developed and implemented, such as Problem-Based Learning. These strategies intend to help students develop cognitive, instrumental, and attitudinal skills (Knowledge, Skills, Attitudes), among others, as structuring elements to ensure the quality and safety of their clinical practice. Quality and safety in clinical practice are associated with intrinsic and extrinsic factors for healthcare professionals. Of the intrinsic factors, clinical decision-making skills stand out. The development of clinical decision-making skills in healthcare students is one of the biggest challenges posed to higher education institutions teachers [3]. This becomes more evident in pre-graduate training with students without clinical experience. In addition, from a student's point of view, this is also one of the main challenges faced. Learning in the healthcare field implicates the need to ensure the quality and safety of the decision in each action, usually linked to fear of making mistakes, causing harm to the patient and, consequently, likely to negatively impact students’ mental health [4,5,6,7]. Thus, it is crucial to develop, implement and evaluate strategies that enable or recreate clinical environments and clinical decision scenarios before tutored or autonomous clinical practice. These environments must recreate spaces of high realism and fidelity creating friendly learning environments and recreating emotionally safe but simultaneously challenging spaces where students can build their learning [8].
The educational strategies traditionally used in health have almost reached their highest potential, thus stimulating innovation through new andragogical strategies that support the interaction of those involved in learning in enhancing active learning and capturing the intrinsic motivation of students, directing them to the translation of knowledge, enabling more meaningful learning, and leading to greater perception of effectiveness and less likelihood of clinical error [3, 8].
In the last decades, simulation in health has emerged as a pedagogical strategy whose evidence demonstrates improved knowledge retention, instrumental, relational and communication skills, leadership and teamwork skills, and the transference of competencies [9,10,11].
Clinical virtual simulation
Currently, the technological development in information and communication technologies allows to recreate patients and clinical conditions in virtual learning environments. These virtual patients are computer programs that simulate real-life clinical scenarios in which students act as health professionals, collecting the clinical history, performing the physical examination, defining the diagnosis, the intervention to be implemented, and evaluating the outcome of the clinical decision. Virtual simulation is defined as a type of simulation that places the student at the centre of decision-making, motor and/or communication skills [12].
The use of virtual patients in a virtual healthcare environment to train clinical reasoning and/or clinical decision-making skills has been defined as clinical virtual simulation (CVS) [13, 14]. Using virtual patients in education effectively improves knowledge, critical thinking, clinical reasoning, instrumental skills, self-efficacy perception, learning satisfaction, interaction and feedback, teamwork, learning experience, and realism of simulation spaces, making them emotionally safer [13, 15,16,17,18,19,20,21,22,23,24].
The increased use of clinical virtual simulation in recent years in health education was boosted during and after the COVID-19 pandemic. Despite the recognition achieved during these pandemic years, little is known about the factors that influence the acceptance by students of the use of clinical virtual simulation.
In 2016, the Nursing School of Porto began developing clinical virtual scenarios in Nursing to be integrated into the clinical virtual simulator Body Interact® (BY).
The use of clinical virtual simulation in the Nursing Degree as an andragogical strategy began in 2018–2019. Since then, studies have been conducted on usability [13, 25], knowledge retention, satisfaction and learning perception [14], the impact on learning in small groups, and the perception of curricular integration [26].
However, further investigation is needed regarding the factors that promote the adoption and use of clinical virtual simulation by students. The use of clinical virtual simulation as an integrated pedagogical strategy in a health degree implies the reorganization of the curricular plans and the introduction of andragogical strategies directed to enhancing active learning and capturing the intrinsic motivation of the student to learn [8].
The technology acceptance model
In technology and education, the Technology Acceptance Model (TAM) is a theoretical model that predicts the acceptance of the use of technology by users [27]. This model was developed by Davis F.D. (1989) [28], to which were added the determinants of perceived utility by Davis & Venkatesh (2000) [29] and the determinants of ease of use by Venkatesh V. (2000) [30]. More recently, Venkatesh V. & Bala H. (2008) developed an integrated Technology Acceptance Model 3 (TAM3) including a structure of the individual determinants for the adoption and use of technology.
Based on the TAM3 [31], this study sought to identify the factors/determinants that predict the use of clinical virtual simulation in nursing education.
Methodology
An observational, cross-sectional, analytical study of the use of clinical virtual simulation was carried out to answer the research question: What factors/determinants predict the acceptance and use of a clinical virtual simulator in nursing education? (Table 1).
Selection of participants
All students of the 2nd, 3rd, and 4th year of the Nursing Degree in the Nursing School of Porto (ESEP) (n = 870) were invited to participate in this study.
Considering all items related to TAM, with a count of 62 items, and applying the rule of thumb suggested by Nunnally (1978) [32] of 10 cases per variable, the recommended sample size would be 620 participants.
Following a non-probabilistic sampling methodology, a convenience sample of nursing students was selected, who voluntarily agreed to participate, and following the inclusion/exclusion criteria:
Inclusion criteria: ESEP degree students who completed attendance, with or without success, of the curricular unit Body Responses to Disease 1 (RCD 1) in the academic years 2019–2020, 2020–2021, and 2021–2022.
Exclusion criteria: ESEP degree students who have not attended the curricular unit Body Responses to Disease 1 in the academic years 2019–2020, 2020–2021, and 2021–2022, and students who obtained accreditation to the curricular unit.
In our study, the actual sample size is n = 619 participants. It's important to note that we do not conduct a unified analysis for all 62 items. Therefore, our sample size is similar to the calculated requirement, providing a robust foundation for the statistical analyses employed in our study.
Ethical considerations
The ESEP’s ethics committee granted authorisation for the study 697/2022 and informed consent was obtained from all participants.
Data collection
Data were collected through a questionnaire adapted from the Technology Acceptance Model 3 [31, 33].
The variables under study are defined in Tables 2 and 3.
For the translation and validation into European Portuguese of the Technology Acceptance Model 3, authorization was granted from the authors and the following steps were carried out [33, 34]:
-
1.
Stage I – Initial translation
-
a.
Translation 1 from English into Portuguese performed by a professional Portuguese native translator (without knowledge of the TAM3);
-
b.
Two translations by Portuguese native speakers, one trained in the field of Computer Sciences (without knowledge of the TAM3) (Translation 2) and one healthcare professional with experience using the TAM3 and clinical virtual simulation (Translation 3), both proficient in English.
-
a.
-
2.
Stage II—Synthesis of translations Translation 1, 2 and 3
-
a.
Production of the Translation final version 1 (Researcher, two native Portuguese speakers, one from the health area with experience in the use of clinical virtual simulation and the TAM3 and another from the area of Computer Sciences—different from the participants in stage I);
-
a.
-
3.
Stage III—Back-translation by two English native speakers (without medical background).
-
4.
Stage IV—Analysis by an expert group with experience in the use of the TAM3 and virtual simulation in nursing education
-
a.
Semantic equivalence (adapted to the clinical virtual simulation);
-
b.
Ideological equivalence;
-
c.
Experiential equity;
-
d.
Conceptual equivalence.
-
a.
-
5.
Stage V—Pre-test of the pre-final version with a group of 10 students who were not included in the study sample.
-
6.
Final version—The authors waived submission of the version for evaluation and approval.
Data were collected between May and July 2022.
Data analysis
In the initial phase, frequencies and descriptive statistics were extracted from all the collected variables. This approach allowed the analysis of the distribution of variables, evaluating the sensitivity of items (used to evaluate latent constructs) and detecting potential atypical values (outliers). Then, the Shapiro–Wilk test was used to assess the normality of the distribution of variables, and values of asymmetry and kurtosis were used to assess the degree of separation of variables from normal distribution. The main psychometric properties of the different dimensions of the TAM3 were studied. Different validity criteria (criterion and construct validity) were applied considering best practices [35] and the evaluation of their internal consistency. To evaluate the constructs internal to the TAM3 and external (individual determinants), exploratory factor analysis (EFA) was performed to define the factors associated with the constructs of the TAM3. Subsequently, confirmatory factor analysis (CFA) was employed to verify whether the items of each scale saturated the identified factors. Path analysis was used to determine the main predictors (and relevant interactions between predictors) of the intention to use clinical virtual simulation in learning, the main dependent variable to model. This analysis included other variables besides its immediate predictors, such as the perceived usefulness and perceived ease of use. Different mediation models were also developed to test whether some of the explored variables inhibited the relationship between the most relevant variables of the TAM3.
The data related to the global score variables of utilization (GS) and system utilization (SU) were extracted from the Learning Management System (LMS) of the clinical virtual simulation. The global score variable refers to the average overall evaluation obtained by the student in clinical virtual simulation utilization regarding his/her clinical decision-making skills, measured in percentage of success. The system utilization variable (SU) refers to the total number of clinical scenarios the student completed in the clinical virtual simulation.
Statistical analysis was performed using JASP, Jamovi, IBM SPSS Amos v.26, and IBM SPSS Statistics v. 26. The results are reported following the APA standards, presenting the magnitude measurements of the Cohen d effect (0.2 low; 0.5 medium, and 0.8 high) and considering of P < 0.05 as significant. In the confirmatory factor analysis, the criteria applied to evaluate the adjustment of the model were the χ2 value and its p-value, ideally nonsignificant, the CFI > 0.95, GFI > 0.90 and RMSEA > 0.03 and < 0.08 [36]. In the analysis of the convergent validity of the items internal to the TAM3, the reliability value of the construct (CR) > 0.8, the mean extracted variance (AVE) > 0.5 [36], and factor loads in inter-correlation items lower than the square root of the AVE for each construct were the adopted criteria [37].
Results
A total of 619 Nursing students participated in this study, being 85.50% (n = 531) female, 35.1% (n = 218) 2nd-year students; 36.2% (n = 225) 3rd-year students; and 28.7% (n = 178) 4th-year students. Table 4 presents the descriptive statistics of the sample, and Table 5 the correlation matrix of age, course marks, number of completed scenarios and mean global evaluation score.
Analysis of the acceptance of the use of CVS by the TAM3
Descriptive analysis of the items, followed by the exploratory factor analysis (EFA), confirmatory factor analysis (CFA), and trajectories analysis, were performed sequentially to investigate the acceptance of the use of the CVS and to identify the factors that determine the acceptance and use of the clinical virtual simulation in nursing education, as presented below.
Descriptive analysis of the items of the TAM3
The descriptive results of the Technology Acceptance Model 3 items, organised according to the constructs internal to the TAM and the individual determinants (constructs external to the TAM).
Exploratory factor analysis of the TAM
After the descriptive analysis of the data, the internal constructs associated with the Technology Acceptance Model 3 (PU-perceived usefulness; PEOU-perceived ease of use and BI-Behaviour intention to use) were analysed. Firstly, the EFA, using the Axis Factoring Main method, the Oblimin rotation method and the Kaiser Normalization criterion (KMO = 0.894, and Bartlett’s sphericity test < 0.001) were applied to analyse whether the items presented adequate factor loadings in each construct of the Technology Acceptance Model 3. The EFA allowed to identify three factors associated with the internal constructs of the Technology Acceptance Model 3 that explain 74.6% of the total variance of the data and present an adequate internal consistency (Table 6).
Then, EFA was performed with the items of individual determinants of the TAM3 (e.g., CSE-Self-efficacy in the use of CVS; PEC-Perception of external control; CPLAY-Perceived playfulness in the use of CVS; CANX-Anxiety with the use of CVS; ENJ-Enjoyability associated with the use of CVS) to analyse whether the items revealed adequate factor loadings in each individual determinants of the TAM3. In the EFA, the principal axis factoring method was used with the Oblimin rotation, and the Kaiser Normalization criterion for factor extraction. To analyse the adequacy of the data to perform the EFA, the Kaiser–Meyer–Olkin test (KMO) was performed considering a value greater than 0.8 as meritorious [38] and the Bartlett’s Sphericity test p < 0.05 to test the relationship between the variables (KMO = 0.879; Bartlett’s sphericity test < 0.001). The EFA allowed to identify ten factors that explained 59.4% of the total variance of the data. However, items OUT_2_TAM34; CANX_1_TAM13; CPLAY_4_TAM47; PEC_4_TAM12; SN_3_TAM22; SN_4_TAM23; CPLAY_4_TAM47; PEC_4_TAM47; PEC_4_TAM12; SN_TAM23; SN_4_TAM3; SN_TA3; SN_2_TA3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM33; SN_2_TAM3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM_TAM3; SN_TAM3; SN_TAM33; SN_TAM3; SN_TAM3 presented factor loadings < 0.3 [36] or cross factor loadings in more than one factor, so they were excluded from the analysis. We performed a second EFA excluding the problem items described (KMO = 0.867; Bartlett’s sphericity test < 0.001). This analysis allowed to identify eight factors that explain 68.64% of the variance of the data. However, we verified that items PEC_2_TAM10, PEC_3_TAM11, and PEC_1_TAM9 had factor loadings < 0.3 or cross-factor loadings in more than one factor, so they were excluded from the analysis. Excluding these items, we performed a new EFA (KMO = 0.856; Bartlett’s Sphericity test < 0.001) that identified 7 factors, explaining 63.1% of the total variance of the data and presenting adequate internal consistency (Table 7).
Confirmatory factor analysis of the TAM
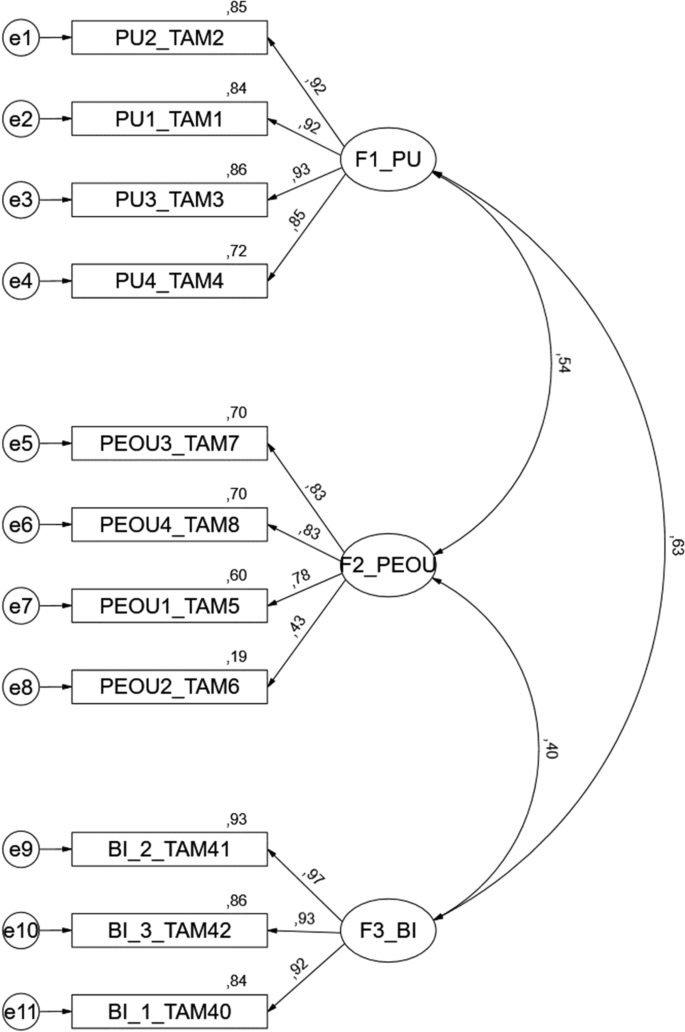
Once the factorial structure of the Technology Acceptance Model 3 was defined for this study, a confirmatory factor analysis (CFA) was performed to validate the constructs internal to the Technology Acceptance Model 3 (Perceived usefulness, Perceived ease of use, and Behaviour intention to use), although ideally, this analysis requires a new sample. The results revealed acceptable adequacy of the model (Fig. 1) [(χ2(41) = 178, P < 0.001, CFI = 0.976, PCFI = 0.727, GFI = 0.948; PGFI = 0.589, RMSEA = 0.075; p(rmsea 0.05) < 0.001)]. Table 8 presents the results of the construct’s validity.
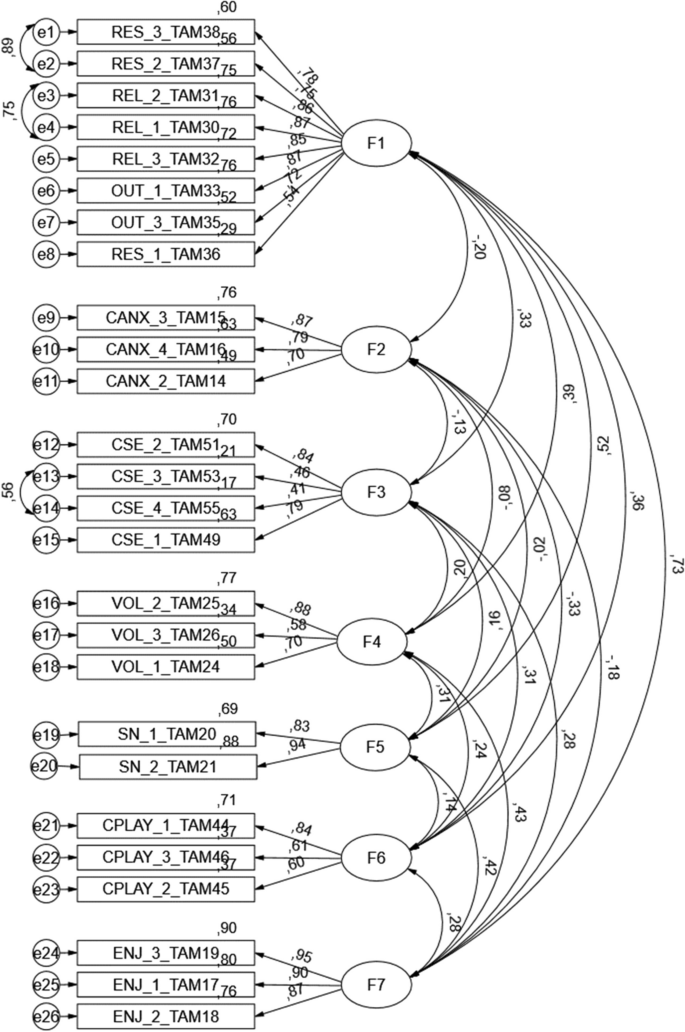
The analysis of Table 9 shows the appropriateness of convergent and discriminant validity of the proposed model (Fig. 1). CFA was performed to validate the constructs associated with the determinants external to the Technology Acceptance Model 3 (REL-Relevance for learning; CANX-Anxiety with the use of CVS; CSE-Self-efficacy in the use of CVS; VOL-Voluntariness; PEC-Perception of external control; SN-Subjective Norm; CPLAY-Perceived playfulness in the use of CVS; ENJ-Enjoyability associated with the use of CVS) (Fig. 2). The results showed an acceptable fit to the model [(χ2(275) = 621, P < 0.001, CFI = 0.949, PCFI = 0.803, GFI = 0.888; PGFI = 0.695, RMSEA = 0.057; p(rmsea 0.05) = 0.025)]. Table 10 shows the construct validity results, with all items, except CSE_4_TAM55, presenting factorial loads greater than 0.5, revealing an acceptable convergent validity [36].
CFA model of the individual determinants of TAM 3. Footnote: F1-REL-Relevance to learning; F2—CANX—Anxiety with the use of CVS; F3—CSE—Self-efficacy in the use of CVS; F4—VOL—Voluntariness; F5—SN—Subjective Norm; F6—CPLAY—Perceived Playfulness in the use of CVS; F7—ENJ—Enjoyability associated with the use of CVS
The errors of the items with higher modification index values were correlated to improve the adjustment of the model. More specifically, a correlation was established between the following items: RES_3_TAM38 and RES_2_TAM37; REL_2_TAM31 and REL_1_TAM30; CSE_3_TAM53, and CSE_3_TAM55. This decision was based on the content similarity presented by the correlated items.
The convergent validity of the individual determinant items of the TAM3, a Construct Reliability (CR) revealed a value greater than 0.73, an Average Extracted Variance (AVE) greater than 0.42 [36], and factorial loadings in the inter-item correlation lower than the square root of the AVE for each construct [38], highlighted bold in Table 11 above the diagonal. The global analysis indicates the appropriateness of convergent and discriminant validity of the proposed model.
Trajectory analysis
In the proposed model, the items’ global average score of evaluation of the use of the virtual simulator (GS) and those related to the use of clinical virtual simulation (SU) were not considered (Table 12), given the high number of missing values (higher than 30%) that negatively influenced data quality and weakened the proposed model. The high number of missing values is justified by the participation in this sample of 4th-year students who attended the curricular unit Body Responses to Disease 1 in 2019–2020, an academic year in which it was not possible to extract the variables per student from the LMS.
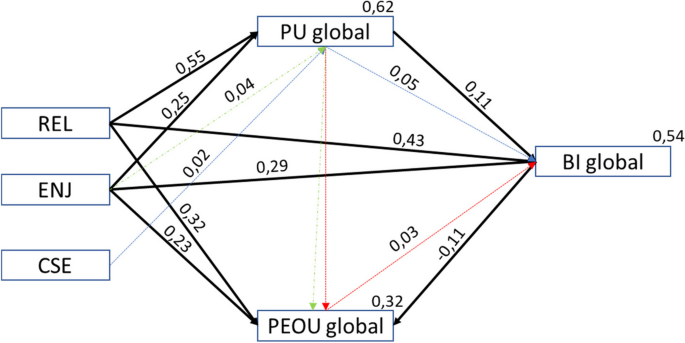
Trajectory analysis was used to analyse the adequacy of the TAM3 adapted to assess the acceptance of the use of clinical virtual simulation. Table 13 summarises the tested hypotheses. Figure 3 represents the standardised constructs coefficients of the model and coefficients of determination (R 2) associated with the modelling of the dependent variables. The model presents values of [(χ2(5) = 7.22, p = 0.205, CFI = 0.999, PCFI = 0.111, GFI = 0.998; PGFI = 0.091, RMSEA = 0.027; p(rmsea 0.05) = 0.789)]. In Fig. 3, the proposed model explains a high variance of perceived usefulness (R 2 = 62%), intention to use the CVS (R 2 = 54%), and a lower variance of ease of use (R 2 = 32%).
Table 13 shows that the defined hypotheses related to the internal constructs and the individual determinants of the TAM3 regarding the acceptance of the clinical virtual simulation, the perceived usefulness (PU), the perceived ease of use (PEOU) and the behaviour intention to use (BI)], are influenced by Relevance for learning (REL) [REL → PU (β = 0.55; P < 0.001), REL → PEOU (β = 0.32; P < 0.001), REL → BI (β = 0.43; P < 0.001)], and Enjoyability (ENJ) [ENJ → PU (β = 0.25; P < 0.001), ENJ → PEOU (β = 0.23; P < 0.001), ENJ → BI (β = 0.29; P < 0.001)]. The remaining hypotheses were not supported in this study.
Table 14 shows the standardised indirect effects of the Model proposed for the acceptance of the technology for CVS (TAM3CVS_MP).
Discussion
The participants showed mean values of perceived usefulness (M = 5.34; SD = 1.19), ease of use (M = 4.74; SD = 1.07), and behaviour intention to use the clinical virtual simulation (M = 5.21; SD = 1.18), indicating the acceptance of the use of clinical virtual simulation in nursing education.
This study validated the use of the Technology Acceptance Model 3 adapted to clinical virtual simulation and tested the related hypotheses, showing that the model explains 62% of perceived usefulness, 32% of ease of use, and 54% of behaviour intention to use the clinical virtual simulation by nursing students. The adequacy of the model was tested by analysing the direct effects of the relationships between the internal constructs (PU → BI, β = 0.11, P = 0.012; PEOU → BI, β = -0.11, P = 0.002) and direct relations between some of the constructs internal to the TAM and the external determinants, Relevance for learning and Enjoyability. Also, the adequacy of the proposed model was determined by analysing the indirect effects of self-efficacy in the use of clinical virtual simulation (CES) on BI (P = 0.05) through PU (P = 0.02) and the indirect effect on Enjoyability (ENJ) on PU through PEOU (P = 0.044) and the indirect effect of PU on BI through PEOU (P = 0.026).
In sum, regarding the technology acceptance model for clinical virtual simulation, the internal constructs that predicted the intention to use were perceived usefulness and perceived ease of use. However, perceived ease of use emerges as new its inverse relationship with the behaviour intention to use. This fact finds no parallel in the evidence [33, 39,40,41,42,43]. This data points out that the responses expressed by the students are not related to the ease of use inherent to technology but rather to the cognitive performance necessary for the resolution of clinical scenarios and the training of clinical decision-making skills. Thus, the greater the perception of ease of use in a perspective of greater competence in the clinical decision-making process, the lower the intention to use the clinical virtual simulation. These data also reveals the need for clinical scenarios to present an increasing level of complexity according to the development of clinical decision-making skills.
In the proposed model, Relevance for learning (REL) and Enjoyability (ENJ) were the external constructs that best predicted perceived usefulness, ease of use, and behaviour intention to use clinical virtual simulation. This is in line with some of the findings of a meta-analysis by Rosli M.S et al. (2022) [43], the study of the adequacy of the Technology Acceptance Model 3 to virtual reality by Jiang, M et al. [39], and the study on the acceptance of computer games as an educational strategy, where Relevance for learning was also identified as one of the best predictors of perceived usefulness and/or ease of use by Lemay, D. J et al. [41].
The decision on the behaviour intention to use the clinical virtual simulation should consider three indirect effects identified:
-
The self-efficacy in the use of the clinical virtual simulation (CVS) indirectly predicts the behaviour intention to use the CVS through the moderation of perceived usefulness. This emphasises the need to optimise the support to students with less perceived self-efficacy in the use of CVS;
-
Enjoyability predicts ease of use of CVS through moderation of perceived usefulness. This fact points to the perception of enjoyability having a positive influence on the perceived usefulness, which positively influences the ease of use of the CVS. Also, this demonstrates that the increased Enjoyability associated with use can help overcome some of the complexity perceived by the student in the use of CVS;
-
The perceived usefulness predicts the behaviour intention to use CVS through moderation of perceived ease of use. These data point out that a greater utility perceived by the student in the use of CVS helps overcome some of the complexity perceived in the use of CVS in clinical reasoning training.
The analysis of the descriptive data associated with each construct internal to the TAM3 and the individual determinants showed average scores ranging between 4.14–5.59, except for Anxiety related to the use of the CVS, with an average score of 1.5, indicating its low perception by the students. The average self-efficacy score of the use of CVS (M = 6.72) is explained by the fact that it is evaluated on a 10-point Guttman scale. The lowest average score observed is for the subjective norm, indicating that it is not the influence of other people, particularly teachers, that determined the use of CVS by students. Regarding the voluntary use of CVS, data should be interpreted with caution since items TAM25 (M = 4.71) and TAM26 (M = 4.34) revealed a low perception of obligation perceived by the student to use the CVS, while item TAM24 (M = 5.24) showed a higher value associated to the voluntary use of the CVS. Regarding the ease of use, item TAM6 (M = 4.06) revealed that the use of CVS did not require much effort, as opposed to item TAM7 (M = 5.10), expressing the ease of use.
These are innovative results as they highlight the positive influence that the relevance attributed to learning and development of clinical reasoning and clinical decision-making skills (Learning Relevance) have on the perception of ease of use, perceived usefulness in the use of CVS, and the effective use of CVS. These results are associated with the relevance attributed by the student who views the use of CVS as linked to the triggering of emotions such as enjoyability, a fact previously determined as a variable to adjust the use of technology by Venkatesh V. & Bala H. (2008) [31] but still little explored by Kim, S et al. [44]. This study shows that the use of CVS, ease of use, and usefulness are influenced by the positive representation that the student has of the contribution to their training as a future nurse. Also, these study results demonstrate that the use of CVS creates a playful context that helps students learn actively in a friendly environment, bringing aspects of gamification that help them set goals, get scores, and compare results between students [44, 45] while simultaneously anticipating clinical challenges. Using game elements added to the CVS contributes to developing intrinsic motivation [46] and satisfaction with the learning process [8].
The use of CVS promotes students’ active learning and the capture of their intrinsic motivation through facilitated access to pedagogical resources according to the pacing and learning preferences of the students. This learning environment promotes autonomy, the development of effectiveness and belonging to a learning community, an environment in which the teacher is a facilitator of the learning process, and the student learns while having fun [46,47,48]. It can be argued that the motivation under analysis can be extrinsic [46] because it uses a perception of locus of internal causality associated with an integrated regulation process by anticipating the results that students may achieve, a fact represented by the construct Relevance for learning (REL). However, the construct Enjoyability clarifies the existence of intrinsic motivation based on interest and student satisfaction with the learning process using the CVS [46]. Thus, this study showed that a personal determinant of the student (REL) and an adjustment determinant (ENJ) are central to the use of CVS in nursing education.
Currently, the acceptance and adoption of CVS in Nursing education, in this context, goes beyond external variables to the student that may determine the adoption of CVS, for example, the influence of teachers and significant people or individual determinants related only to characteristics of CVS, for example, the effectiveness in the use of CVS, anxiety associated with the use of CVS, and playfulness. This study revealed that the current characteristics of pre-graduation students, who are digital natives [49], lead to features related to the use of technology that may be overcome by the nature of the learning outcomes anticipated by students.
In sum, this study produced interesting outcomes for nursing education in this context, affirming that the use of CVS in learning is directly determined by students’ perceived relevance and enjoyability. This positively influences the usefulness and perceived ease of use and consequently the behaviour intention to use the CVS. Perceived Self-efficacy indirectly predicted the behaviour intention to use CVS through moderation by perceived usefulness.
The results of this study require careful interpretation because they only represent a single context of nursing degree education and were implemented in one of the curriculum units of the syllabus. Notwithstanding, this study presents data that can support educators in the health field in making decisions or developing new studies, overcoming some of the limitations of this study.
Study limitations
The main limitations of this study were the use of the same sample of students to perform the EFA and CFA.
Another identified limitation was not having included the construct of the attitude referred to in other studies. This option was based on the expectation of having data related to the behaviour from the evaluation and use of the CVS. Also, the lack of data for the entire sample regarding the Global Scores of use and the number of completed scenarios per student conditioned the potential of the presented model. Thus, using this model in samples with these available data is recommended. This limitation stems from the fact that CVS is still little used as an andragogical strategy in health education.
Conclusion
This study provided noteworthy contributions to propose a technology acceptance model for clinical virtual simulation (TAM3CVS_MP), identifying the factors determining the acceptance and use of clinical virtual simulation by nursing students.
The results showed the potential of clinical virtual simulation as a pedagogical strategy to capture students' intrinsic motivation to develop active and optimised learning while potentiating their skills.
Integrating clinical virtual simulation as an andragogical strategy in nursing education curriculums needs to rely on higher education institutions and teachers, investment in training, technology and time for reflection, discussion, and analysis. However, this study provides information that can support the decision and shape the implementation strategy.
Furthermore, this study evidences the importance of teachers’ and institutional decision-makers’ attention to students' perception of relevance for learning, enjoyability, and perceived self-efficacy associated with the use of clinical virtual simulation during conceptualisation, design, and implementation processes.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author but restrictions apply to the availability of these data, which were used under license from the Nursing School of Porto (Portugal) for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from Nursing School of Porto (Portugal).
Abbreviations
- AVE:
-
Average extracted variance
- BI:
-
Behaviour intention to use
- CANX:
-
Anxiety with the use of CVS
- CFA:
-
Confirmatory factor analysis
- CPLAY:
-
Playfulness in the use of CVS
- CR:
-
Construct reliability
- CSE:
-
Self-efficacy in the use of CVS
- CVS:
-
Clinical virtual simulation
- ECTS:
-
European credit transfer and accumulation system
- EFA:
-
Exploratory factor analysis
- ENJ:
-
Enjoyability associated with the use of CVS
- ESEP:
-
Nursing School of Porto
- GS:
-
Global score
- HEIs:
-
Higher education institutions
- IMG:
-
Image
- KMO:
-
Maiser-Meyer-Olkin test
- LMS:
-
Learning management system
- OU:
-
Objective usability
- OUT:
-
Evaluation result
- PEC:
-
Perception of external control
- PEOU:
-
Perceived ease of use
- PU:
-
Perceived usefulness;
- RCD 1:
-
Body responses to disease 1 course
- REL:
-
Relevance for learning
- RES:
-
Learning relevance
- SN:
-
Subjective norm
- SU:
-
CVS use
- TAM:
-
Technology acceptance model
- VOL:
-
Voluntariness
References
Wensing M. Grol R. Knowledge translation in health: how implementation science could contribute more. BMC Med, 2019;8(17). https://doi.org/10.1186/s12916-019-1322-9.
Légaré F. Zhang P. Barriers and facilitators - Strategies for identification and measurement. (J. T. Sharon E. Straus, Ed.) Knowledge translation in health care: moving from evidence to practice. 2013
Berman NB, et al. The Role for Virtual Patients in the Future of Medical Education. Acad Med. 2016;91(9):1217–22. https://doi.org/10.1097/ACM.0000000000001146.
Ruud N. et. al. Comparing mental distress and help-seeking among first-year medical students in Norway: results of two cross-sectional surveys 20 years apart. 2020;10. doi:https://doi.org/10.1136/bmjopen-2020-036968.
Mao Y. et al. A systematic review of depression and anxiety in medical students in China. 2019;19. https://doi.org/10.1186/s12909-019-1744-2.
Moreira S.J. et. al.Anxiety, Depression and Academic Performance: A Study Amongst Portuguese Medical Students Versus Non-Medical Students. Acta Med Port, 2018 ;28(31(9)), pp. 454–462. doi:https://doi.org/10.20344/amp.9996.
Karaca A, et al. Relationship between mental health of nursing students and coping, self-esteem and social support. Nurse Educ Today. 2019;76:44–50. https://doi.org/10.1016/j.nedt.2019.01.029.
Padilha, J. M., Rosa, J. L., & Cunha, D. J. Gamification in Healthcare Education: Demystifying a Trend. Em B. Oscar, V. Amorim, & A. C. Moreira, Handbook of Research on the Influence and Effectiveness of Gamification in Education. IGI Global. 2022. doi:https://doi.org/10.4018/978-1-6684-4287-6.ch003.
Shin S et al.. Effectiveness of patient simulation in nursing education: Meta-analysis. 2015;35(1), pp. 176–182. Doi.https://doi.org/10.1016/j.nedt.2014.09.009.
Vlachopoulos D. Makri A. The effect of games and simulations on higher education: a systematic literature review. Int J Educ Technol High Educ, 2017;14(22). https://doi.org/10.1186/s41239-017-0062-1.
Moslehi S, Masoumi G, Barghi-Shirazi F. Benefits of simulation-based education in hospital emergency departments: A systematic review. J Educ Health Promot. 2022. https://doi.org/10.4103/jehp.jehp_558_21.
-Lioce L. (Ed.) et al. Healthcare Simulation Dictionary - Seconde edition. 2020.doi:https://doi.org/10.23970/simulationv2.
Padilha JM, et al. Clinical Virtual Simulation in Nursing Education. Clin Simul Nurs. 2018. https://doi.org/10.1016/j.ecns.2017.09.005.
Padilha JM, et al. Clinical Virtual Simulation in Nursing Education: Randomized Controlled Trial. J Med Internet Res. 2019. https://doi.org/10.2196/11529.
Pence, P. L. Student satisfaction and self-confidence in learning with virtual simulations. Teaching andLearninginNursing, 2022;31–35. doi:doi.org/https://doi.org/10.1016/j.teln.2021.07.008.
Plackett, R., Kassianos, A. P., Mylan, S., Kambouri, M., Raine, R., & Sheringham, J. The effectiveness of using virtual patient educational tools to improve medical students’ clinical reasoning skills: a systematic review. BMC Medical Education, 2022;1–18. doi:https://doi.org/10.1186/s12909-022-03410-x.
Sim JJ, Rusli KD, Seah B, Levett-Jones T, Lau Y, Liaw SY. Virtual Simulation to Enhance Clinical Reasoning in Nursing: A Systematic Review and Meta-analysis. Clin Simul Nurs. 2022;69:26–39. https://doi.org/10.1016/j.ecns.2022.05.006.
Brown K.M. et al. Integrating Virtual Simulation into Nursing Simulation Roadmap. Clinical Simulation in Nursing, 2021; pp. 1-9. https://doi.org/10.1016/j.ecns.2021.08.002.
Dale-Tam J. et. al. Creating Psychological Safety During a Virtual Simulation session. Clinical Simulation in Nursing, 2021; pp. 14–17. doi:https://doi.org/10.1016/j.ecns.2021.01.017.
Foronda C.L. et. al. Virtual simulation in nursing education: a systematic review spanning 1996 to 2018. Simulation in Healthcare 2020;(15), pp. 46–54. doi:https://doi.org/10.1097/SIH.0000000000000411.
Fogg N, et al. Using virtual simulation to develop clinical judgment in undergraduate nursing students. Clin Simul Nurs. 2020;48:55–8. https://doi.org/10.1016/j.ecns.2020.08.010.
Kyaw B.M. et. al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J Med Internet Res, 2019; 21(1). doi:https://doi.org/10.2196/12959.
Kononowicz A. et. al. Virtual Patient Simulations in Health Professions Education: Systematic Review and Meta-Analysis by Digital Helath Education Collaboration. J Med Internet Res, 2019; 21(7). doi:https://doi.org/10.2196/14676.
Baumann-Birkbeck L. et. al. Appraising the role of the virtual patient for therapeutics health education. Curr Pharm Teach Learn, 2017;9(5), pp. 934–944. doi:doi: https://doi.org/10.1016/j.cptl.2017.05.012. Epub
Padilha JM, et al. Clinical Virtual Simulation as Lifelong Learning Strategy—Nurse’s Verdict. Clin Simul Nurs. 2020. https://doi.org/10.1016/j.ecns.2020.06.012.
Mestre A, Muster M, El Adib AR, Egilsdottir HÖ, Byermoen KR, Padilha J, M.,… Marreiros, A. The impact of small group virtual patient simulator training on perceptions of individual learning process and curricular integration: a multicentre cohort study of nursing and medical students. BMC Med Educ. 2022. https://doi.org/10.1186/s12909-022-03426-3.
Granić A, Marangunić N. Technology acceptance model in educational context: A systematic literature review. Br J Edu Technol. 2019;50(5):2572–93. https://doi.org/10.1111/bjet.12864.
Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of infrmation technology. MIS Q. 1989;19:319–40.
Venkatesh V. Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manag Sci. 2000;46:186–204.
Venkatesh V. Determinants of perceived ease of use: integrating perceived behavioral control, computer anxiety and enjoyment into technology acceptance model. Inf Syst Res. 2000;342–65.
Venkatesh V. Bala H. Technology Acceptance Model 3. 2008;39(2), pp. 273–315. doi:https://doi.org/10.1111/j.1540-5915.2008.00192.x.
Nunnally JC. Psychometric theory. 2nd ed. New York: McGraw-Hill; 1978.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine. 2000;25(24):3186–91.
Boateng et. al.Boateng GO, Neilands TB, Frongillo EA, Melgar-QuiñoBest Practices for Developing and Validating Scales for Health, Social, and Behavioral Research: A Primer. Front Public Health, 2018; 6(49). doi:https://doi.org/10.3389/fpubh.2018.00149.
Hair JF Jr, Black WC, Babin BJ, Anderson RE. Multivariate data analysis (7. th. New York: Pearson; 2010.
Fornell C, Larcker DF, (Feb de,. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J Mark Res. 1981;18(1):39–50.
Kaiser, H. F. An index of factorial simplicity. Psychometrika, 1974; 31–36. doi:https://doi.org/10.1007/BF02291575.
Fussell SG, Truong D. Using virtual reality for dynamic learning: an extended technology acceptance model. Virtual Reality. 2022;26:249–67. https://doi.org/10.1007/s10055-021-00554-x.
Jiang, M. Y.-C., Jong, M. S.-Y., Lau, W. W.-f., Meng, Y.-l., Chai, C.-S., & Chen, M. Validating the General Extended Technology Acceptance Model for E-Learning: Evidence From an Online English as a Foreign Language Course Amid COVID-19. Front. Psychol., 2021;12. doi:https://doi.org/10.3389/fpsyg.2021.671615.
Huang Y-M. Exploring students’ acceptance of educational computer games from the perspective of learning strategy. Australas J Educ Technol. 2019;35(3):132–49. https://doi.org/10.14742/ajet.3330.
Lemay DJ, Morin MM, Bazelais P, Doleck T, (July de,. Modeling students’ perceptions of. Clin Simul Nurs. 2018;20:28–37. https://doi.org/10.1016/j.ecns.2018.04.004.
Abdullah F, Ward R. Developing a General Extended Technology Acceptance Model for E-Learning (GETAMEL) by analysing commonly used external factors. Comput Hum Behav. 2016;56:238–56. https://doi.org/10.1016/j.chb.2015.11.036.
Rosli, M. S., Saleh, N. S., Ali, A., Bakar, S. A., & Tahir, L. M. A Systematic Review of the Technology Acceptance Model for the Sustainability of Higher Education during the COVID-19Pandemic and Identified Research Gaps. Sustainability, 2022; 14. doi:https://doi.org/10.3390/su141811389.
Kim, S., Song, K., Lockee, B., & Burton. Gamification in Learning and education - Enjoy Learning Like Gaming. Springer International Publishing AG. 2018. doi:https://doi.org/10.1007/978-3-319-47283-6.
-van Gaalen, A., Brouwer, J., Schönrock-Adema, J., Bouwkamp-Timmer, T., Jaarsma, A., & Georgiadis, J. (May de,. Gamification of health professions education: a systematic review. Adv Health Sci Educ Theory Pract. 2021;12:683–711. https://doi.org/10.1007/s10459-020-10000-3.
Ryan, R. M., & Deci, E. L. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. American Psychologist, 2000.pp. 68–78. doi:10.1037110003–066X.55.1.68
Kusurkark RA, Croiset G, Ten Cate TJ. Twelve tips to stimulate intrinsic motivation in students through autonomy-supportive classroom teaching derived from self-determination theory. Med Teach. 2011. https://doi.org/10.3109/0142159X.2011.599896.
Ten Cate, O. T., Kusurkar, R. A., & Williams, G. C. How self-determination theory can assist our understanding of the teaching and learningprocesses in medical education. AMEE Guide No. 59. Medical Teacher, 2011;33(12), pp. 961–973. doi:https://doi.org/10.3109/0142159X.2011.595435.
Prensky, M. Digital Natives, Digital Immigrants Part 1. 2001; 9(5), pp. 1–6. doi:https://doi.org/10.1108/10748120110424816.
Acknowledgements
The authors wish to acknowledge the contribution of the professional translator Maria do Amparo Alves on the editing of this article.
Funding
None declared.
Author information
Authors and Affiliations
Contributions
All authors conceived the study. JMP collected, prepared, and analysed the data with PC. All authors confirm that they had full access to all the data in the study, take responsibility for the integrity of the data and the accuracy of the analysis, and accept responsibility to submit the paper for publication. JMP drafted the initial and final versions of the manuscript. All authors critically revised the early and final versions of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Nursing School of Porto ethics committee granted authorisation for the study 697/2022 and informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Descriptive analysis of the TAM item.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Padilha, J.M., Costa, P., Sousa, P. et al. Clinical virtual simulation: predictors of user acceptance in nursing education. BMC Med Educ 24, 299 (2024). https://doi.org/10.1186/s12909-024-05154-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05154-2