- Research
- Open access
- Published:
A feasibility study of a handmade ultrasound-guided phantom for paracentesis
BMC Medical Education volume 24, Article number: 351 (2024)
Abstract
Background
Simulation-based training is effective for ultrasound (US)-guided procedures. However, commercially developed simulators are costly. This study aims to evaluate the feasibility of a hand-made phantom for US-guided paracentesis.
Methods
We described the recipe to prepare an agar phantom. We collected the US performance data of 50 novices, including 22 postgraduate-year (PGY) residents and 28 undergraduate-year (UGY) students, who used the phantom for training, as well as 12 emergency residents with prior US-guided experience. We obtained the feedback after using the phantom with the Likert 5-point scale. The data were presented with medians and interquartile ranges (IQRs) and analyzed by the Wilcoxon rank sum test.
Results
While emergency residents demonstrated superior performance compared to trainees, all trainees exhibited acceptable proficiency (global rating of ≥ 3, 50/50 vs. 12/12, p = 1.000) and comparable needle steadiness [5 (5) vs. 5 (5), p = 0.223]. No significant difference in performance was observed between PGYs [5 (4–5)] and UGYs [5 (4–5), p = 0.825]. No significant differences were observed in terms of image stimulation, puncture texture, needle visualization, drainage simulation, and endurance of the phantom between emergency residents and trainees. However, experienced residents rated puncture texture and draining fluid as “neutral” (3/5 on the Likert scale). The cost of the paracentesis phantom is US$16.00 for at least 30 simulations, reducing it to US$6.00 without a container.
Conclusions
The paracentesis phantom proves to be a practical and cost-effective training tool. It enables novices to acquire paracentesis skills, enhances their US proficiency, and boosts their confidence. Nevertheless, further investigation is needed to assess its long-term impact on clinical performance in real patients.
Trial registration
NCT04792203 at the ClinicalTrials.gov.
Introduction
Clinical procedures involve a complex combination of technical skills and cognitive decision-making. Achieving expert performance and sustaining skills necessitate deliberate practice [1]. Traditionally, procedural skills were acquired, and experience accumulated through direct application on real patients. However, concerns about patient safety and rights have escalated with inexperienced physicians performing procedures directly on patients. Simulation-based medical education provides an alternative for skill proficiency [2], particularly in ultrasound (US)-guided procedures [3].
Paracentesis is a commonly encountered procedure in clinical practice. The use of ultrasound guidance diminishes the risk of a dry tap (failure to obtain fluid) during paracentesis and reduces the likelihood of complications such as bleeding, abdominal hematoma, and puncture site infection [4, 5]. Additionally, US-guided procedures are integral to emergency medicine training [6]. However, commercially developed simulators for US-guided procedures are often prohibitively expensive for many emergency departments.
An increasing number of low-cost, handmade phantoms have been developed for US-guided biopsy, thoracocentesis, and pericardiocentesis [3, 7,8,9,10,11,12,13,14,15,16,17]. However, options for paracentesis remain limited [18,19,20]. Furthermore, more evidence is needed to assess the learning impact of using handmade phantoms for paracentesis training. This study aims to evaluate the feasibility of a handmade phantom for US-guided paracentesis.
Methods
This prospective study was conducted at the Emergency Department of the National Taiwan University Hospital (NTUH) from August 2022 to July 2023. It was approved by the institutional review board of the NTUH (202011111RIND) and registered at ClinicalTrials.gov (NCT04792203). Informed consent was obtained from each participant.
Phantom preparation
-
1.
Agar substrate
The agar substrate was created by dissolving 10 g of agar powder in 1000 cc of water. After thorough heating to melt the agar powder, the solution underwent filtration to remove impurities. The resulting clear solution was tinted with dark blue food coloring additives.
-
2.
Paracentesis phantom
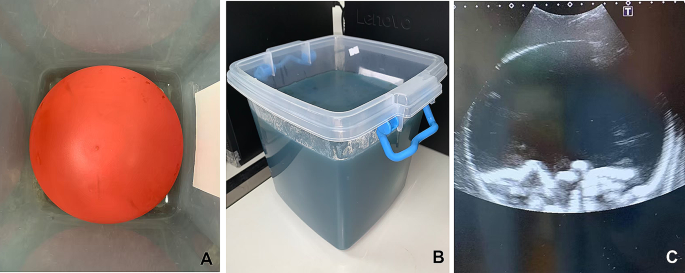
A cotton rope, at least 30 cm in length, was inserted into a 10-inch balloon to simulate the bowel. The balloon was then filled with yellowish water dyed with food coloring additives to mimic ascites. After tying the balloon securely, it was affixed to the bottom of the container using super glue (Fig. 1A). The balloon was covered with the agar substrate, replicating the appearance of human skin and the subcutaneous area. The thickness of the covering could be adjusted based on different body habitus. The phantom was refrigerated for a minimum of 4 h to enhance its longevity (Fig. 1B).
The resulting phantom exhibited easily distinguishable echogenic structures (Fig. 1C, Supplementary Video). The balloon effectively delineated boundaries between the peritoneum and the subcutaneous area.
US-guided paracentesis using the hand-made phantom
We recruited 50 trainees, comprising 22 postgraduate-year 1 (PGY-1) residents and 28 undergraduate-year (UGY) students, for participation in a US training curriculum. To assess their experience and confidence in using US, the trainees completed a survey using a 5-point Likert scale (1 = not confident at all; 2 = slightly confident; 3 = somewhat confident; 4 = fairly confident; 5 = completely confident). Subsequently, they attended a 30-minute didactic session covering the theory of US and US-guided paracentesis, followed by small-group hands-on training utilizing the agar phantom. The instructors, were certified by the Taiwan Society of Emergency Medicine.
Following the curriculum, all trainees underwent a skill test, performing paracentesis. The performance was evaluated using an assessment form (Table 1) in which the items of the assessment was developed to to encompass the training domains based on expert consensus. Three experts, certified by the Taiwan Society of Emergency Medicine and with over 10 years of US experience, participated in establishing this consensus.
Two independent evaluators, not involved in enrollment and training, graded the performance—one on-site, and the other assessed video recordings with trainee faces masked. Subsequently, trainees provided feedback on the phantom through a survey using a 5-point Likert scale (Supplementary Table 1).
Additionally, 12 emergency residents were enrolled to use the phantom without didactics and hands-on training. Their performance was graded, and a survey regarding the phantom was collected.
US machines (Xario 100, Canon, Japan, and Arietta 780, Fujifilm Healthcare, Japan) equipped with a 2–5 MHz curvilinear transducer were used.
Statistical analysis
All data were analyzed by SAS software (SAS 9.4, Cary, North Carolina, USA). Initially, we conducted the Shapiro-Wilk test to assess the normality of continuous data. If the data did not follow a normal distribution, it was presented using medians and interquartile ranges (IQRs). For the comparison between residents and trainees, as well as between PGYs and UGYs, we employed Wilcoxon’s rank-sum test.
To assess inter-rater reliability between two evaluators for the items on the assessment form and global scores, we utilized the intraclass correlation coefficient (ICC) with 95% confidence intervals (CIs). The Spearman correlation coefficient was used to evaluate the relationship between the total score and the global score. The total score represented the sum of each item on the assessment form. The internal reliability of the assessment form was estimated by employing Cronbach’s alpha coefficient [21]. A p-value less than 0.05 was considered statistically significant.
Results
Following the assessment of normality, it was determined that the scores for each item on the assessment form, the global score, and feedback to the phantom were not normally distributed (all p < 0.0001). Therefore, these data were reported using medians and IQRs.
US performance
The 50 trainees were all considered US novices (Table 2). The 12 emergency residents had previous experience with US-guided paracentesis on more than 20 real patients. The ICC for the global score was 0.94 (95% CI, 0.90–0.96), indicating strong inter-rater reliability, as was observed for the items on the checklist (Supplementary Table 2). The Spearman correlation coefficient was 0.79 (95% CI, 0.67–0.87) between the total score and the global score, indicative of strong correlation. The standardized Cronbach’s alpha coefficient was 0.75, suggesting good internal reliability.
While the performance of emergency residents surpassed that of trainees, all trainees demonstrated acceptable performance (global rating of ≧ 3). Trainees exhibited less familiarity with US-guided localization, visualization of the needle, and fluid aspiration (Table 2). No significant differences were found in the performance between PGYs and UGYs (Supplementary Table 3).
Phantom
There were no significant differences observed in terms of image stimulation, puncture texture, needle visualization, drainage simulation, and endurance of the phantom between emergency residents and trainees. However, it is noteworthy that the residents rated puncture texture and draining fluid as “neutral (Table 3). Trainees reported increased confidence in paracentesis after using the phantom, compared with their pre-curriculum survey [4 (3–5) vs. 1 (1), p < 0.0001].
The US phantom could be utilized at least 30 times for practicing paracentesis within one curriculum. The cost of the handmade phantom with a container was approximately $16. Without the container, the cost was reduced to approximately $6.
Discussion
Commercial US phantoms for paracentesis remain extremely expensive rendering them inaccessible for many training centers. Inexpensive, do-it-yourself phantoms play a crucial role in paracentesis training. In this study, we presented a low-cost, and easily reproducible phantom with echogenicity similar to human tissue and proved its feasibility. Utilizing the phantom facilitates the acquisition of paracentesis skills among novices, enhancing their US abilities and boosting their confidence. While novices demonstrated acceptable performance in paracentesis, it still lags behind that of experienced residents.
Apart from their higher cost, commercial phantoms may degrade with repeated use, requiring an additional fee for fixation. These phantoms typically incorporate polymers, resulting in an excessively firm texture. In contrast, our agar phantom, while having a semi-firm texture that may not perfectly replicate human skin, received a median rating ranging from 3 to 4 from experienced emergency residents in terms of feedback, encompassing image stimulation, puncture texture, needle visualization, and drainage simulation.
Reviewing the literature, some examples of inexpensive, handmade paracentesis phantoms were reported. Wilson et al. documented a gelatin phantom [18], and Kei et al. employed a water jug covered with pork belly [20]. Mesquita et al. used multiple gloves filled with various colors to simulate ascites and abdominal organs, elucidating students’ perceptions of the simulator [19]. In our study, we contribute additional evidence supporting the viability of a handmade phantom, reporting on the performance and feedback of novices in comparison to experienced residents.
Moreover, our phantom exhibited variability and flexibility. For instance, the fluid within the phantom could be altered to appear red or include debris content (such as adding talc), replicating hemoperitoneum or pus, respectively. Additionally, the ratio of fluid to ropes could be adjusted to simulate either a small or a large amount of ascites, depending on the desired training difficulty.
Lower-fidelity modalities are designed to concentrate on a specific learning task and skill acquisition, making them suitable for early learners or novices. In contrast, higher-fidelity simulations are employed for complex tasks, providing cognitive stimuli [1]. Our handmade phantom is a tool with lower fidelity in external appearance but exhibits high fidelity in ultrasound appearance, making it well-suited for paracentesis training, with novices demonstrating proficiency after completing the curriculum. It is important to note that the long-term impact on skill retention and the translation of acquired skills to proficiency in clinical settings remains unknown.
Gelatin is frequently employed as the primary substrate for homemade phantoms in ultrasound training [12, 18, 22]. However, gelatin necessitates refrigeration to solidify the model. In contrast, agar serves as a vegan-friendly alternative that can set the model without the need for refrigeration. Agar is capable of producing an ultrasound image that closely mimics real tissue and is durable enough to withstand high-volume training [23]. In this study, we opted for agar as the substrate, and the resulting echogenicity was deemed acceptable.
The assessment form was developed through expert consensus to ensure content validity. Our results also demonstrated good internal and interrater reliability of the assessment form. Research indicates that global rating scales effectively capture various proficiency levels compared to checklists and are user-friendly for examiners [24]. In this study, the global rating score was utilized to evaluate performance in conjunction with the items on the assessment form.
The main limitation of this study was the inclusion of trainees and emergency residents from a single institution, who voluntarily participated and exhibited high motivation, potentially introducing selection bias. Therefore, caution should be exercised when generalizing these results. Secondly, the study involved a substantial amount of labor and time, approximately 30–60 min for agar preparation and an additional 30 min for phantom assembly, which could limit its feasibility due to time constraints. Third, there may be a potential issue with the image quality of the phantom, as a small amount of air might have been introduced into the balloon during fluid aspiration. However, both trainees and residents reported acceptable image quality. Fourth, while the trainees had prior experience in blood drawing and needle catheterization through routine medical training, feedback concerning human tissue and draining sensation should be interpreted cautiously. Notably, residents with real-world experience rated “neutral” on aspects such as “puncture texture mimics human skin and subcutaneous area” and “draining fluid is realistic.” Lastly, the focus of this study was on evaluating the feasibility of the phantom. Factors such as skill retention and the clinical performance of trainees in real-world scenarios were not investigated. Additionally, the learning effect of using handmade phantoms was not compared with that of using commercial phantoms due to the latter’s high cost. These aspects should be addressed in future studies.
Conclusion
The paracentesis phantom proves to be a practical and cost-effective training tool. It facilitates the acquisition of paracentesis skills among novices, enhancing their US abilities and boosting their confidence. Nevertheless, further investigation is needed to assess its skill retention and long-term impact on clinical performance in real patients.
Data availability
All data analyzed during this study are included in this published article.
Abbreviations
- Ultrasound:
-
US
- National Taiwan University Hospital:
-
NTUH
- Postgraduate-year:
-
PGY
- Undergraduate-year:
-
UGY
- Interquartile range:
-
IQR
- Intraclass correlation coefficient:
-
ICC
- Confidence interval:
-
CI
References
Wang EE, Quinones J, Fitch MT, Dooley-Hash S, Griswold-Theodorson S, Medzon R, Korley F, Laack T, Robinett A, Clay L. Developing technical expertise in emergency medicine–the role of simulation in procedural skill acquisition. Acad Emerg Med. 2008;15(11):1046–57.
Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40:254–62.
Giannotti E, Jethwa K, Closs S, Sun R, Bhatti H, James J, Clarke C. Promoting simulation-based training in radiology: a homemade phantom for the practice of ultrasound-guided procedures. Br J Radiol. 2022;95(1137):20220354.
Patel PA, Ernst FR, Gunnarsson CL. Evaluation of hospital complications and costs associated with using ultrasound guidance during abdominal paracentesis procedures. J Med Econ. 2012;15(1):1–7.
Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013;143(2):532–8.
ACEP. Ultrasound guidelines: Emergency, Point-of-care and clinical Ultrasound guidelines in Medicine. Ann Emerg Med. 2017;69(5):e27–54.
James V, Kee CY, Ong GY. A homemade, high-fidelity Ultrasound Model for simulating pneumonia with Parapneumonic Effusion and Empyema. J Emerg Med. 2019;56(4):421–5.
Sullivan A, Khait L, Favot M. A novel low-cost ultrasound-guided Pericardiocentesis Simulation Model: demonstration of feasibility. J Ultrasound Med. 2018;37(2):493–500.
Fredfeldt KE. An easily made ultrasound biopsy phantom. J Ultrasound Med. 1986;5(5):295–7.
McNamara MPJ, McNamara ME. Preparation of a homemade ultrasound biopsy phantom. J Clin Ultrasound. 1989;17(6):456–8.
Silver B, Metzger TS, Matalon TA. A simple phantom for learning needle placement for sonographically guided biopsy. AJR Am J Roentgenol. 1990;154(4):847–8.
Wilson J, Myers C, Lewiss RE. A low-cost, easy to make ultrasound phantom for training healthcare providers in pleural fluid identification and task simulation in ultrasoundguided thoracentesis. Visual J Emerg Med. 2017;8:80–1.
Do HH, Lee S. A low-cost training Phantom for Lung Ultrasonography. Chest. 2016;150(6):1417–9.
Zerth H, Harwood R, Tommaso L, Girzadas DV Jr. An inexpensive, easily constructed, reusable task trainer for simulating ultrasound-guided pericardiocentesis. J Emerg Med. 2012;43(6):1066–9.
Daly R, Planas J, Edens M. Adapting Gel Wax into an ultrasound-guided pericardiocentesis model at low cost. Western J Emerg Med. 2017;18(1):114–6.
Young T, Kuntz H. Modification of Daly’s Do-it-yourself, Ultrasound-guided pericardiocentesis model for added external realism. Western J Emerg Med. 2018;19(3):465–6.
DIY Ultrasound Phantom Compendium. [https://www.ultrasoundtraining.com.au/resources/diy-ultrasound-phantom-compendium/)].
Wilson J, Wilson A, Lewiss RE. A low-cost, easy to make ultrasound phantom for training healthcare providers in peritoneal fluid identification and task simulation in ultrasound-guided paracentesis. Visual J Emerg Med. 2017;8:29–30.
de Mesquita DAK, Queiroz EF, de Oliveira MA, da Cunha CMQ, Maia FM, Correa RV. The old one technique in a new style: developing procedural skills in paracentesis in a low cost simulator model. Arq Gastroenterol. 2018;55(4):375–9.
Kei J, Mebust DP. Realistic and Inexpensive Ultrasound Guided Paracentesis Simulator Using Pork Belly with Skin. JETem 2018, 3(3):127–132.
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334.
Aytaç BG, Ünal S, Aytaç I. A randomized, controlled simulation study comparing single and double operator ultrasound-guided regional nerve block techniques using a gelatine-based home-made phantom. Med (Baltim). 2022;101(35):e30368.
Earle M, Portu G, DeVos E. Agar ultrasound phantoms for low-cost training without refrigeration. Afr J Emerg Med. 2016;6(1):18–23.
Rajiah K, Veettil SK, Kumar S. Standard setting in OSCEs: a borderline approach. Clin Teach. 2014;11(7):551–6.
Acknowledgements
We thank the Ministry of Science and Technology, Taiwan (MOST 110-2511-H-002-009-MY2) for financial support.
Funding
The Ministry of Science and Technology (MOST 110-2511-H-002-009-MY2).
Author information
Authors and Affiliations
Contributions
CT and WC conceived the study and designed the trial. CT, CH, SY, SS, and WC acquisition of the data. CT and WC analysis and interpretation of the data. CT and WC drafted the manuscript, and all authors contributed substantially to its revision. WC critically revised the manuscript for important intellectual content and took responsibility for the paper as a whole. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the Research Ethics Committee of the National Taiwan University Hospital (202011111RIND). Informed consent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, CT., Lin, CH., Lin, SY. et al. A feasibility study of a handmade ultrasound-guided phantom for paracentesis. BMC Med Educ 24, 351 (2024). https://doi.org/10.1186/s12909-024-05339-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05339-9